Introduction

Hi, I’m Anthony. I walk barefoot 🦶 , I sleep on the floor 💤 and I exclusively eat meat 🥩 . Needless to say, I’m fairly unconventional.
Friends of mine will tell you that I’m a joyful, stoic, kind, humble and easygoing young man – although some claim that I’m really 90 years old. I’m inquisitive and enjoy riddles, problem solving and the daily crossword – indeed, 90 years old. I strive to live a fulfilling, low-stress, happy life. 😊
Health has long been an important value to me ever since I was a little Anthony. I feel and preform my best physically, mentally and emotionally when I prioritize my health and well-being. A few years ago, however, I was shocked to learn that what I thought was a healthy diet was in fact a big fat lie.
The purpose of this website is to open your eyes to the industry influence, statistical manipulation and biased recommendations that are all-to-common in today’s nutritional guidelines. I’ll also introduce you to the proper human diet, backed by over one hundred research papers, books and historical references. It goes against almost everything you’ve been taught about nutrition, and it works.
Get ready to unlearn everything you know about nutrition.
So who pays you to promote this? I am not financially endorsed or influenced by any organization or industry, nor am I making any money from this website. It’s sole purpose is to share my passion and informed opinions on health. This website is the result of thousands of hours of independent research, reading, writing and programming.
I know, I should probably get a life.
You're Being Fed Lies
Nutrition Research Is Nearly All Rubbish,
Big Food Influences & Shapes Our Dietary Guidelines,
Eat Less, Move More Is Worthless Weight Loss Advice,
Calories Don’t Matter,
Eating Fat Doesn’t Make You Fat,
Saturated Fat Won’t Give You Heart Disease,
Cholesterol Won’t Clog Your Arteries,
Meat Doesn’t Give You Cancer,
Fruits & Vegetables Are Not Essential for Optimal Health,
Vegetarian & Vegan Diets Are Inferior to Meat Diets,
Salt Doesn’t Lead to Heart Disease...
...You're Being Fed Lies!
"People are fed by the food industry which pays no attention to health, and treated by the medical industry which pays no attention to food."
– Wendell Barry, American novelist
The food industry’s largest constituents (Big Food) make hundreds of billions of dollars a year selling you "food". These highly profitable foodstuffs almost always consist of dirt cheap grains, sugars and/or seed oils. Coincidentally, these are three of the most harmful ingredients to your health – and most addicting to the palate.
Do you really think that Nestle, Kellogg's and Kraft actually care about your health?
These food giants – not to mention the billion dollar diet and supplement industry – would crumble into bankruptcy if people knew true health. Their one and only objective is to sell you "food" and pills; whether they’re actually healthy or not is irrelevant to them.
The more processed garbage they convince you to buy, the more money they make. These mega-corporations have a huge financial incentive in ensuring that what they sell is deemed "healthy" – or at least not harmful to your health.
The Push For Profits Plants
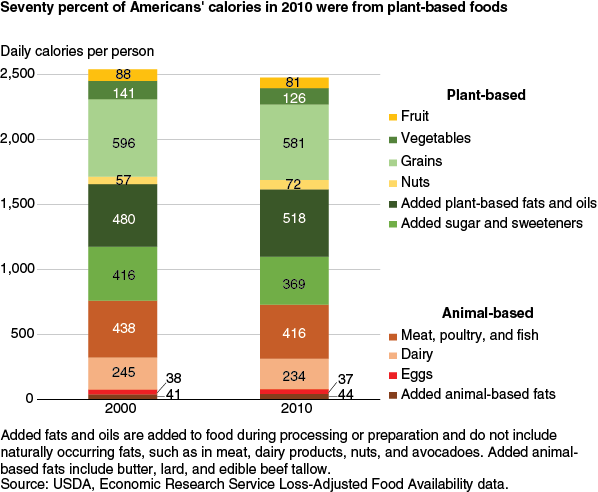
Over the past few years, there’s been a massive push for plant-based diets. Most governments and health agencies around the world condemn the consumption of saturated fat & cholesterol laden animal-foods and heavily promote "heart-healthy" plant-based alternatives.
You would think that these recommendations emerged from considering the totality of nutritional research and forming an objective dietary plan that would best nourish the populous.
Nope. It’s not because plant-based diets are healthier for you. It’s simply because plant-based foods are much more profitable to Big Food than animal-based foods are. As you’ll discover in the research section below, many health agencies around the world are sponsored by and financially supported by – therefore influenced by – Big Food. Like the answer to most of society’s questions : Follow the money.
Trusting Big Food with health advice is like trusting a casino with financial advice.
Consider the Beyond Burger : a pea protein isolate, expeller-pressed canola oil, rice protein, plant-based patty (with 15 other oddly named ingredients). This concoction of processed powders and oils is supposedly healthier than a plain, natural beef patty?
Diets Suck
Essentially all well known diets revolve around caloric reduction and fat phobia. Yet there is ample evidence that low calorie and low-fat diets do not work. Sure, they might lead to some temporary weight loss, but at what cost?
- Relentless hunger,
- Irritable behaviour,
- Low energy,
- Tasteless food,
- Tracking food intake,
- Guilt from not achieving your target goals...
...All so that you regain your lost weight a few weeks later – and then some. This isn’t a sustainable or enjoyable way to live a life.
Fortunately, there is a diet that is easy and enjoyable to follow, without any of the downsides of traditional dieting. It gives you all the nourishment your body requires, improves energy levels, mental focus, mood, strength, digestion and sleep – just to name a few. If anything, weight loss is an added bonus.
It’s not a "fad diet". It’s not "the new quick fix". It’s how our sapien ancestors have been eating for millions of years. It’s what has allowed us as a species to become the most intelligent life-form on this planet (well, some of us anyway.)
The Proper Human Diet
Unfortunately the term diet has a bad rap. It’s usually seen as a short term fix to lose a few pounds, and rarely as a long-term lifestyle. In my mind, a diet is a template that helps you prioritize the consumption of nourishing foods and limit unnourishing foods (or "non-foods" as I prefer to call them).
So what is the proper human diet?
Meat.
That’s it!? Yea, that’s it.
To the contrary of what is advised by Canada’s Dietary Guidelines, I currently eat copious amounts of red meat, saturated fat and sodium – and have been doing so for almost 3 years now – and I’ve never felt better. (Other than the occasional vegan aggression.)
Meat and animal sourced foods – beef, pork, chicken, eggs, dairy and fish – provide your body with all of the essential vitamins, minerals, amino-acids and fatty acids that the body needs to thrive. In fact, adopting an animal-based / meat / carnivore diet has resolved many "incurable" ailments in some who have tried it. Revero.com has compiled hundreds of success stories from people who are now disease free and thriving thanks to the proper human diet.
You likely have more questions than answers at this point. I’ve created an FAQ section below which may address some of your concerns and inquiries. Otherwise, you can always send me a message and I will be happy to answer your individual question, or in the least point you to a resource on the topic.
– Anthony, "The Meat Guy"
#eatmeat #meatheals #carnivorediet
FAQs
Find answers to (some of) your questions. Visit the research section for studies cited in the FAQ section.
What Does "Nutrire" Mean?

Nutrire : latin for 'to nourish'
\ nūtrīre \
- to be nourishing, to be nutritious;
- to supply with what is necessary for life, health, and growth;
- to sustain with food or nutriment.
Nourish your being with the nutrients it needs. Feed your soul with energy and positivity. Take care of the one and only body you have on this earth. Seek purpose, fulfillment and joy.
Yearn to thrive, not just exist.
What's an Animal-Based / Meat / Carnivore Diet?

In simple terms, it’s the opposite of a vegan diet. Meat, eggs, fish and dairy make up the bulk this diet.
The carnivore diet is a diet in which you exclusively consume animal sourced foods. Animal-based (like myself) prioritize animal sourced foods, but allow small amounts of non-animal sourced foods. (Coffee, tea, spices, mushrooms, certain vegetables, the occasional sweet treat...)
Animal sourced foods are incredibly nutrient dense, meaning that you get much more nutrition per meal than you would on a vegan diet for example. Animal protein is an especially underrated nutrient that most people could use more of.
Because the selection of food is quite limited, some use it as an "elimination diet" to pin point food intolerances.
How Is It Different Than Other Diets?

Unlike traditional diets, there is :
- NO calorie counting,
- NO pills or powders,
- NO tracking intake,
- NO relentless hunger,
- NO energy crashes, and
- NO mood swings.
All while indulging on nourishing, delicious, fatty, juicy meat. And it works!
Unlike a "starvation" diet, a carnivore diet nourishes and satiates your body with all of the essential nutrients vital to good health. It helps reset your hunger hormones, so you’ll naturally be less hungry if you have excess stored fat you can burn as fuel.
It’s well documented in the scientific literature that calorie restriction does NOT lead to significant long term weight loss.
The carnivore diet works on a principle other than calories. By heavily reducing or eliminating carbohydrates in your diet, your fat storing hormone (insulin) will drastically drop. This in turn will allow your body to use dietary fat as a fuel source and will allow your fat cells to release their stored fat. Essentially, you turn into a fat burning machine, without feeling starved.
Who Invented It?

It’s nothing new. Our sapien ancestors started consuming meat over a million years ago. Since then, our brain size tripled in size.
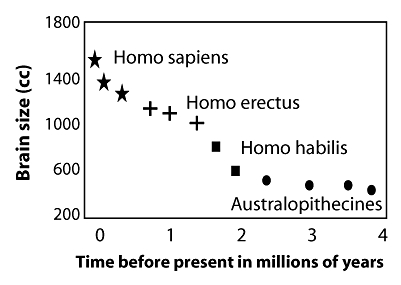
Meat has been a major part of our diet for hundreds of thousands of years, and is what has made us the most intelligent lifeforms on this planet.
As for the diet itself, it dates as far back as 150 years. A man named William Banting was urged to try a meat heavy diet for his obesity and sluggishness after having failed calorie restrictive diets from his doctor. He admits that he has "never lived so well as under the new plan of dietary."
Why Diet if I'm Already Thin?

As many as 7 out of 8 (87.8%)of Americans are metabolically unhealthy, even in normal weight individuals.
Weight is only one of many markers of good health. Other markers to look out for are :
- Blood sugar levels,
- Insulin levels,
- Triglycerides levels,
- Visceral fat (fat within the abdomen and in the organs),
- Blood pressure,
- Oxidized LDL,
- Mental health,
- Energy levels,
- Sleep quality.
You may have a normal body weight, but hidden within may be signs of ill-health.
Additionally, although exercise has many great benefits, you cannot out-exercise a bad diet. It will catch up to you eventually. I personally know a fit, thin man in his 40’s who runs marathons regularly, and was diagnosed with type 2 diabetes. (Also vegetarian, which doesn’t help.)
How Will a Meat Diet Improve My Health?

Most people assume that health issues just appear with age – that they’re genetic and inevitable. However, diet and lifestyle plays a huge role in your current and long-term health – yes, even mental health.
Almost any health condition you can think of – skin issues, digestive issues, mental issues, sleep issues, allergies, arthritis, low-energy, obesity, diabetes, etc... – are either improved or completely cured on a carnivore diet. It’s almost unreal how powerful this diet is at healing "incurable" ailments. Revero.com has an impressive collection of testimonials from those who have greatly benefited from a carnivore diet.
Many of those who were taking life-long prescription drugs either cut back substantially on their doses, or eliminated their prescription entirely.
For some, it’s a way to deal with food and sugar addiction – a condition that most people refuse to admit they have.
Oh, and as an added bonus, it will help you lose weight. (Although I disagree that weight alone is the best indicator of health.)
Is It Complicated?

Here’s the complete guide to following a carnivore diet :
Are You Hungry?

Do You Have Animal Products To Eat?

Is It Tastefully Seasoned With Salt?

Eat Until You're Not Hungry Anymore.
Salt to taste.
It's really that simple. No portioning. No calculations. Just nutrient dense animal sourced foods.
Isn't All the Meat, Fat and Salt Going to Kill Me?

I hate to tell you, but you’re going to die of something someday.
Admittedly, there has been very little research done on the long-term effects of a carnivore diet. It’s impossible to say with certainty whether this is a safe and healthy diet to maintain long-term. However, there is very little research on the long-term effects of ANY diet, so you can’t claim that one is safer or healthier than the other.
Some long-term carnivores include Kelly Hogan (12+ years) and Charlene Anderson (20+ years) who are still thriving to this day.
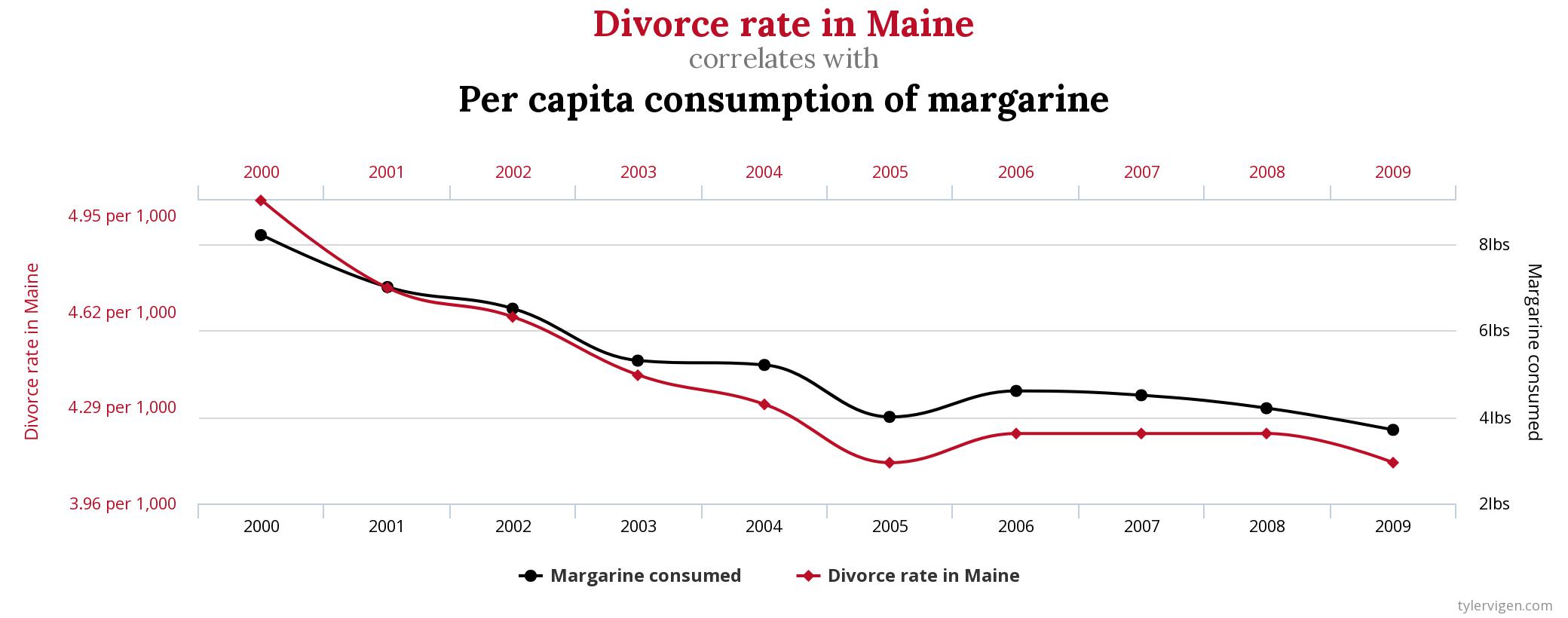
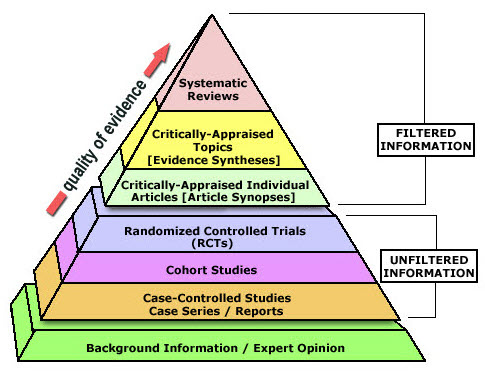
Unfortunately, the field of nutrition research is a total mess. There’s almost never a consensus on any given topic. It’s hard to know what to believe and what to ignore. However, higher quality studies – like some found in the research section – are more telling and trustworthy.
As you’ll discover, saturated fat, animal protein and salt consumption have NO effect on heart disease. Some studies even show an INVERSE association between saturated fat, animal protein and salt intake on mortality.
I have also written detailed articles on the topics of salt, fat, cholesterol and heart disease that can be found in the editorials section.
Elevated insulin appears to be uniquely associated with a number of chronic diseases. Keeping your insulin low via a low-carb or carnivore diet would be my recommendation for a long, healthy, disease-free life.
Aren't Vegetarians and Vegans Healthier Than Meat Eaters?

Despite measures to increase the consumption of fruits, vegetables, whole grains and plant-based proteins, chronic diseases have never been more prevalent.
Now, eating whole, unprocessed foods (either from plant or animal sources) will undoubtedly be healthier for you than consuming processed, refined, multi-ingredient, artificial, industrial box food.
However, there are a number of studies that demonstrate that those who abstain from animal sourced foods have MORE allergies, depression, anxiety, mental health issues and nutritional deficiencies.
In most studies that compare vegetarian diets to "meat" diets, there are a number of factors to take into account :
- There is what’s called a "healthy user bias" among vegetarians. Those who eat a plant-based diet are also more likely to be health conscious. They may consume less sugar, exercise more, drink less alcohol and live a healthier lifestyle than the average person. So in reality, perhaps it’s not their diet which gives them good health, but the other confounding factors.
- Similarly, those who indulge on meat, fat and salt regularly generally disregard health recommendations. They may smoke more, drink more alcohol, eat more processed foods and sugar and generally neglect to take care of their health. So perhaps it isn’t the meat that is causing their ill-health, but the other confounding factors.
- Additionally, based on a USDA report,"meat eaters" are likely eating a diet that only consists of 30% animal sourced foods.
Most people are surprised to learn that you can get all your essential vitamins, minerals and nutrients exclusively from animal sourced foods – even vitamin C. Plants are not essential.
In fact, most plants don’t want to be eaten. They have evolved harmful chemical defences throughout their evolution. These "anti-nutrients" can cause digestive permeability, inhibit the absorption of nutrients, accumulate in the body and even contribute to auto-immune diseases.
Fiber isn’t good for you either. I can assure you that I have no issues with bowel movements without any fiber in my diet. 💩
What About Whole Grains and Complex Carbohydrates?

All complex carbohydrates – such as whole wheat bread, cereal, potatoes and rice – are made up of chains of glucose (sugar) molecules. As they get digested, these chains break down into individual glucose molecules. Meaning that ALL carbohydrates get broken down to simple sugars in the body.
In other words, a whole wheat bun has just as much sugar as a chocolate bar.
Additionally, grains contain a family of anti-nutrients called "lectins", inflammatory proteins that attacks the gut lining, causing "leaky gut."
What About Dietary Supplements?

If a diet requires dietary supplements, it’s simply not a healthy diet. Period.
If, however, you’re looking to get more nutrients in your diet, organ meats are some of the most nutrient dense foods that exist. I consume beef liver (raw even) from time to time for extra nourishment.
What Are the Downsides & Side Effects?

Those who start a carnivore diet (or any diet that lowers carbohydrate intake) may experience the "keto flu" : headache, fatigue, irritability and foggy brain. A number of factors may contribute to these symptoms :
- Sudden Lifestyle Change : Drastically changing your diet from one low in fat to high in fat will inevitably stress your body at first. It usually takes 2-4 weeks for your body to become "fat adapted".
- Dehydration : A low / zero-carbohydrate diet will drastically lower your insulin, which in turn will cause the kidneys to expel more fluids. It’s important to drink more water than usual in the beginning weeks, otherwise symptoms of dehydration may arise.
- Low-Electrolytes : Low insulin will also cause the kidneys to expel more sodium. Low sodium can also contribute to the "keto flu". It’s important to consume generous amounts of salt and other electrolytes while on a carnivore diet. (You can even add some to your water like I do.)
- Food Addiction : Depriving yourself from addictive processed foods and sugar may cause you to experience withdrawal, also contributing to the "keto flu". However, your tastes and cravings will change over time. Today, my palate enjoys steak so much more than ice-cream.
Some downsides include :
- Boredom : Some may find this way of eating very restrictive and get quickly bored of the limited selection of animal-foods. I recommend exploring various cuts of meats, cooking styles and spices that may diversify your meals.
- High Cost : Animal sourced foods tend to be pricier than most plant-based foods. I look at it as a investment towards my long-term health and well-being. Cheaper animal sourced foods – but equally as nutritious – include ground beef, chicken, and eggs.
- Limited Restaurant Selection : Eating out can become more complicated on this diet. Most restaurants offer meat, but often accompanied by non-meat ingredients. Easy options include chicken wings, meatballs or kebabs.
Despite these drawbacks, I believe that the health benefits greatly outweigh the inconveniences. It’s why I’ve stuck to an animal-based diet for almost 3 years now.
What Does Anthony Eat In a Day?

I generally only eat 2 meals a day : breakfast and dinner. Partially out of convenience, and partially because I eat nutrient dense foods that give me plenty of energy for hours at a time. I’m quite an active and muscular guy, so I eat far more than the average person.
Breakfast : 6-8 fried eggs with 6-8 pieces of bacon, or 5-6 sausages.
Dinner : ~2lbs of fatty, well seasoned meat : beef, pork, chicken and/or fish usually.
How Much Protein / Fat / Sodium Does Anthony Eat In a Day?

Honestly, I don’t know. I let me body’s intuition determine how much of what I eat. Like thirst, I drink when I'm naturally thirsty, and stop drinking once I'm sufficiently hydrated.
It only makes sense that your body will naturally crave what it needs to thrive (if eating unprocessed, natural foods of course.) I listen to my body and give it what it needs. I eat when I’m hungry, add salt to taste, and don’t shy away from fat.
What Foods Are Considered "Canivore"?

Any food that comes from an animal :
- Beef,
- Lamb,
- Pork,
- Wild Game,
- Chicken,
- Turkey,
- Duck,
- Eggs,
- Fish,
- Seafood,
- Dairy,
- Organ meats,
- etc...
What Foods Should I Avoid?

Anything processed, especially containing grains, seed oils and/or sugars. Depending on your sensitivity to certain foods, dairy and certain spices could also be no-nos. In the end, it’s up to you to experiment with your tolerances to different foods and add / remove items accordingly.
How Strict Do I Have to Be? Can I Have Cheat Meals?

Going full carnivore is admittedly quite extreme and restrictive. I’m not advocating a 100% meat diet to everyone. However, I think that everyone would benefit from adding more animal sourced protein in their diet.
That said, the occasional sweet treat or carb filled food won’t ruin your health (but might cause food addiction relapse for some.) So go ahead and treat yourself form time to time. Remember that life is short. Memento mori.
Common non-animal sourced food exceptions include coffee, certain spices, apple cider vinegar, fermented / pickled vegetables and mushrooms.
How To Start?

Research : It’s important to know the basics before starting anything. Check out some of the research and resources I’ve provided below. Read some books (The Big Fat Suprise, Sacred Cow). Watch some YouTube nutrition presentations (Low-Carb Down Under, What I've Learned). Follow some of the science.
Set Goals : Continually remind yourself why you want to follow this diet. To regain the physique of your 20 year old self? To wake up feeling refreshed and energized? To run a marathon? To live to be 100? To have more energy to play with your grand-children? To improve your cognitive abilities? Whatever it is, keep track of your progress and continually remind yourself, "why am I doing this?".
Some prefer to go cold turkey (mmm, turkey...), whereas others prefer a gradual transition, adding more and more animal sourced foods in their diet while removing more and more plant foods and carbs. Once adapted to the diet, I would suggest to at least try 2 weeks of pure carnivore just to experience it. Afterwards, if you want to experiment with adding in non-animal sourced foods, be my guest. Do what feels right to you.
Editorials
You've Been Fed A Big Fat Lie – Presentation
March 24th 2021
~ 20 minute watch
Presentation Slides (.pdf)
I had the pleasure of giving a short 20 minute presentation to the Low-Carb / Carnivore Vancouver group. I presented my take on the idea that dietary fat – notably saturated fat and cholesterol – does NOT contribute to heart disease. You can find the link to the video as well as the presentation slides above.
Letter To Health Canada on Sodium Restriction – p.2
February 15th 2021
~ 18 minute read
At the end of January, I was exited to find that Karen from Health Canada had replied to my letter in which I expressed my concerns for the sodium restriction guidelines. (You can find her reply in PDF form above.) She did a poor job at defending her case and failed to convinced me that she was correct in her beliefs. So, I spent over 2 weeks writing her a second, much longer letter (with over 50 citations) to support my case that salt is not culpable in the progression of hypertension, and that insulin may be the missing piece to the puzzle.
Subject : You Have Failed To Prove That Sodium is Culpable For Hypertension
Karen,
Thank you for your detailed and informative response to my previous letter on salt. I appreciate the time you took to elaborate on your position and answer some of the questions I had. Still, I remain unconvinced by your "proof". Most of your claims are baseless and have little significance to the underlying pathology and treatment of hypertension.
Let me ask you Karen, do you personally consume the recommended 1500 mg of sodium every day? Do you meticulously measure every milligram of salt you ingest? If not, it is disgraceful and hypocritical of you to expect the entire country to follow such restrictive and unnatural behaviours – especially since they’re not backed by any quality evidence.
The science is NOT settled. The totality of the evidence has NOT been considered. Your belief that excess sodium consumption causes hypertension is WRONG.
In this subsequent letter, I disprove many of the claims you present in your reply. I also explain in detail a possible causal factor for hypertension – one that has little to do with sodium intake. Once again, I ask you to keep an open mind when reading the following letter. If you truly care about the health of Canadians, please read on.
Hypertension : A Reminder
Hypertension, as defined by the Public Health Agency of Canada, is a state in which "systolic blood pressure [is] at or above 140 mmHg or diastolic blood pressure [is] at or above 90 mmHg." According to the American Heart Association, "essential hypertension (essential in a medical context means idiopathic, that is, of unknown cause) accounts for 95% of all cases of hypertension".
You explain in your response that "[a high sodium intake,] physical inactivity, overweight and obesity, unhealthy diet, harmful use of alcohol, inadequate potassium intake and type 2 diabetes" are all factors that are associated with hypertension.
The "Cause" of Hypertension
As mentioned above, 95% of all cases of hypertension remain a mystery. Apparently though, you claim to know the cause of hypertension. "High blood pressure or hypertension occurs when blood pressure is too high for long periods of time. ... It develops slowly overtime and without obvious symptoms." ...This explains absolutely nothing. These appear to be nothing more than meaningless statements. The only purpose of this explanation is to prove how little you know about hypertension.
Furthermore, you claim that "too much [dietary sodium] can lead to high blood pressure" and that "it is estimated that over 30% of high blood pressure cases in Canada are due to high sodium intake."
This is utterly false.
Upon reviewing the study that this statistic is based on, you grossly misinterpreted the conclusion made in the paper. The authors actually concluded that "reducing dietary sodium additives may decrease hypertension prevalence by 30%."
The report does not mention anywhere that excess sodium intake was responsible for hypertension, simply that reducing sodium intake lowered blood pressure. How are you so certain that excessive alcohol intake, inadequate potassium intake, physical inactivity, obesity, type 2 diabetes, and/or other unknown factors weren't responsible for the the illness?
You cannot interpret studies whatever way you want – especially when public health is at stake. To present this interpretation as fact is misleading, unscientific and is a blatant lie.
Are you really basing dietary guidelines on "estimates", "maybes" and faulty logic? Where is the quality research that supports your position on sodium restriction?
If this same logic used in creating Canada’s dietary guidelines, you may as well scrap the whole thing.
Salt In The Past Century
The prevalence of hypertension has almost quadrupled over the past 80 years. [ref, ref]
Despite the drastic rise in hypertension, the consumption of salt actually went down over the past century. "Our current salt consumption (1.5 to 1.75 teaspoons per day, 8-9 grams) is about one half of the amount consumed between the War of 1812 and the end of World War II, which was about 3 to 3.3 teaspoons (16-17 grams) of salt per day." [ref] Additionally, salt consumption has remained relatively consistent from 1957 to 2003 (mean, 3526 mg/day). How can sodium be blamed for the increasing rate of hypertension, when salt consumption has decreased over the past 2 centuries, and has remained unchanged for the past 50 years?
Thinking about it logically, it doesn’t make much sense that a nutrient that’s been in our environment for hundreds of thousands of years is suddenly responsible for the dramatic rise in hypertension seen in the past century. It much more likely that a new and recent change in our physical or food environment is linked to its etiology.
Problem Solve Like An Engineer
Before even suggesting a solution, engineers are taught to identify the root cause of a problem. This way, they are certain to address the real issue at hand, not just a symptom or a secondary effect.
For example : Ever since you’ve owned it, your hot tub has maintained a comfortable water temperature of 96°F. However, over the past few weeks, the temperature has been slowly and inexplicably creeping up, to the point where it’s now almost unbearably hot. Your first instinct is to add a few trays of ice cubes to the tub. This immediately lowers the temperature and allows you to bathe comfortably again. This solution works for a little while, until the temperature creeps up yet again. This is what is called "treating a symptom".
Indeed, adding ice cubes to the tub will lower its temperature – it’s a working solution. However, it’s far from the most logical. Before even thinking about adding ice cubes to the tub, one should ask : why is the water getting hotter? Could it be that the hot tub is lacking ice cubes? Probably not, as it worked fine before. Or could it be that the temperature regulator is faulty? Ah, now we’re using our brain. The temperature regulator is replaced, and the temperature returns to its comfortable 96°F.
What I’m trying to explain is that just because a solution works (in the short-term), does not mean that the solution was in any way related to the cause of the problem, or that the root issue was addressed. Lowering sodium intake may lower blood pressure (in the short-term), but it does not mean that excessive sodium intake is the root cause of hypertension. Like in my example – and as I’ll explain further on – elevated blood pressure may be caused by a faulty regulator.
This article nicely explains Hill’s criteria for determining causation in statistics.
Treating a Symptom
"Treating a symptom" is unfortunately extremely common in the field of health and medicine. Much of modern medicine is focused on addressing superficial symptoms without having a deep understanding of the underlying issues. With ever increasing specialization in health and medicine, it’s becoming more and more difficult to piece together the sum of the evidence on a given problem. Each is working on their individual piece of the puzzle, yet no one puts the puzzle together. Few of these experts take the time – or are even able – to critically asses the root cause of the problem they’re working on. It’s not that they’re unintelligent, but their specialization bubble prevents them from being able to piece together the totality of the evidence and put the puzzle together.
As an expert yourself, your contribution to the puzzle pertains to the effects of dietary sodium reduction on blood pressure. A somewhat useful piece of information. However, it’s unlikely that you can solve the hypertension puzzle with just this one small piece.
Sodium & Hypertension : A Singled Out Victim
You seem to have forgotten that there are a number of other lifestyle and dietary factors that can also affect blood pressure. I understand that your department focuses primarily on food research, but you seem to focus all of your attention on sodium. I’m curious to know why your emphasis is on sodium restriction and why you essentially ignore the effects of potassium, sugar and alcohol consumption on blood pressure?
You might argue that it’s because "even a modest reduction in dietary sodium can result in a significant decrease in blood pressure." Once again, this statement proves nothing more than your lack of understanding of the effects of sodium on blood pressure.
In this study – the one you referred to in your reply – "reducing dietary sodium additives by 1840 mg/day would result in a decrease of 5.06 mmHg (systolic) and 2.7 mmHg (diastolic) blood pressures." In other words, if you are hypertensive (with blood pressure above 140/90 mmHg), cutting more than half of your sodium intake would only marginally decrease your blood pressure – and likely won’t resolve your hypertension.
In fact, some research suggests that even successfully lowering blood pressure may not even reduce the risk of cardiovascular events. "There were no significant differences in the rates of cardiovascular disease events during follow-up among those assigned vs not assigned to either sodium reduction or weight loss [despite reductions in blood pressure]." [ref] "In even successfully treated hypertensive patients, most CVD events that would have occurred without treatment still occur." [ref]
Where’s The Proof?
Thus far, I have yet to come across any research that proves that excess sodium intake (in isolation) causes hypertension. There doesn’t seem to be a feasible pathological explanation as to why a prolonged, higher than recommended intake of sodium causes hypertension. There are many studies that demonstrate an association between excessive sodium intake and hypertension, but none that prove causality.
Although some studies show that reducing sodium intake reduces blood pressure, it does not imply that excess sodium was responsible for hypertension in the first place. From another point of view, one might think that excess alcohol consumption is the cause of hypertension, since reducing alcohol intake decreases blood pressure similarly to reducing sodium intake.
Research That You Neglected To Review
Although you say that the "totality of best evidence [supports] lowering sodium intake", there appears to be high quality research that contradicts the current sodium guidelines. You have either neglected, ignored, or discarded these studies, since they don’t support your preexisting beliefs.
In this Cochrane Review (one of the most respected and trusted scientific reviews), the researchers conducted a meta-analysis of randomized controlled trials "to assess the long‐term effects of advice and salt substitution, aimed at reducing dietary salt, on mortality and cardiovascular morbidity". The authors of this review concluded that "there is insufficient power to confirm clinically important effects of dietary advice and salt substitution on cardiovascular mortality in nonsensitive or hypertensive populations."
Yet, you claim that "there is evidence for a causal relationship between reductions in sodium intake and all-cause mortality, cardiovascular disease and hypertension". I would love for you to provide me with this high quality evidence.
You mention that "a 2013 Institute of Medicine consensus report found that the methodological quality of studies linking lower sodium intake with adverse health outcomes was variable and this limited the ability to make comparisons or conclusions." (With which I don’t disagree.) However, in the exact same report, the authors conclude that "evidence from studies on direct health outcomes is inconsistent and insufficient to conclude that lowering sodium intakes below 2300 mg per day either increases or decreases risk of CVD outcomes (including stroke and CVD mortality) or all-cause mortality."
Along the same lines, the author of this 2016 scientific paper searched the scientific literature to find any quality research that justifies the current 2300mg/day sodium limit. He concluded that :
- 1. There are no randomized controlled trials (RCTs) allocating individuals to below 2,300 mg and measuring health outcomes;
- 2. RCTs allocating risk groups such as obese prehypertensive individuals and hypertensive individuals down to (but not below) 2,300 mg show no effect of sodium reduction on all-cause mortality;
- 3. RCTs allocating individuals to below 2,300 mg show a minimal effect on blood pressure in the healthy population (less than 1mm Hg) and significant increases in renin, aldosterone, noradrenalin, cholesterol, and triglyceride;
- 4. Observational studies show that sodium intakes below 2,645 mg and above 4,945 mg are associated with increased mortality.
The March 2019 report from the Academy of Sciences on Sodium and Potassium intake concludes that "there remains insufficient evidence to establish sodium [a dietary reference intake] for adequacy."
I think I’ll stop here. If this isn’t proof that your guidelines are baseless, I don’t know what is.
The Wrong Suspect?
I’d like to remind you that "commercially processed foods account for 77% of [Canadian’s] sodium intake." [ref] If those who reduce their sodium intake – likely by decreasing their consumption of processed foods – have lower blood pressure, who’s to say that it’s because of the reduction in sodium (a single nutrient), and not the reduction in processed foods? Perhaps the effect was due to the reduction of processed foods in the diet – notably refined carbohydrates – and had little to do with the reduction of sodium. (Replacing chips with carrots for example.)
Furthermore, you mention that hypertension "develops slowly overtime". It seems more likely that factors that also develop slowly over time (such as obesity, type 2 diabetes, metabolic syndrome or insulin resistance) are more likely to be linked with the progression of hypertension.
Does sodium affect blood pressure? Yes. Is sodium causally responsible for hypertension? Not based on any research I’ve seen. Is there compelling evidence to support an alternative hypothesis for the cause of hypertension? Yes.
The Root Cause of Hypertension?
The cause of essential hypertension remains a mystery and may be multi-factorial. However, there is compelling evidence that insulin may explain its underlying pathology.
Insulin in an anabolic, fat storing hormone and aids in blood sugar regulation. It is well-known that hyperinsulinemia plays an important role in the pathology of obesity [ref, ref, ref, ref] and type 2 diabetes [ref, ref, ref]. Unsurprisingly, there also appears to be an important relationship between elevated insulin levels and hypertension.
First, let’s understand how blood pressure is regulated.
[1] – The Renin-Angiotensin-Aldosterone System (RAAS)
If you are unfamiliar with this system, you should resign now. It is absurd that you are involved in making national dietary guidelines, yet know little to nothing about the diseases you’re trying to prevent.
"The RAAS plays a major role in orchestrating the maintenance of normal blood pressures." [ref] With help from the kidneys, it responds to blood pressure variations and aims to maintain regular blood pressure. This system respond very effectively to low or high blood pressures, and adjusts blood pressure accordingly by retaining or excreting sodium. Pressure natriuresis is the mechanism responsible for excreting excess sodium – along with extracellular fluid – in the urine to lower blood pressure.
"Alterations in the sympathetic nervous system and the renin-angiotensin-aldosterone system are key factors in the development and maintenance of hypertension." [ref] Similar to my hot tub example, it appears that the root issue of hypertension lies in its regulation. Those with obesity tend to have an activated RAAS, which induces hypertension. [ref] Additionally, diabetics are twice as likely to have hypertension as compared to non-diabetics, due to "up-regulation of the renin-angiotensin-aldosterone system, oxidative stress, inflammation, and activation of the immune system." [ref]
[2] – Insulin’s Role in Hypertension
Insulin plays an important role in blood pressure regulation (or deregulation) by promoting the activation of the RAAS. [ref] This is likely why type 2 diabetics – especially those taking exogenous insulin – are more susceptible to hypertension. The following studies serve to support this theory.
In two groups, matched for sex, age, body weight and body fat, "both plasma insulin (50±6 vs. 30±6 μU/mL) and plasma glucose concentrations (114±8 vs. 85±8 mg/dl) at two hours were significantly higher in the hypertensive than in the normotensive subjects." "These results provide preliminary evidence that essential hypertension is an insulin-resistant state." [ref]
Independent of obesity, hypertensives were significantly more insulin resistant. "There was a negative correlation between insulin sensitivity and ... systolic blood pressure." The mean blood pressure and fasting insulin was :
- 125/74 mmHg & 4.7 mU/L for the normotensive group;
- 171/104 mmHg & 7.5 mU/L for the non-obese hypertensive group;
- 168/103 mmHg & 11.9 mU/L for the obese hypertensive group. [ref]
A random population of 2475 individuals were assessed for hypertension and glucose-intolerance. Of the hypertensives, "83.4% ... were either glucose-intolerant or obese – both established insulin-resistant conditions." [ref]
Over a 6 to 12 year follow-up, "subjects with insulin values above the 75th percentile experienced three times more hypertension than did those below the 25th percentile." [ref]
Metabolic syndrome – characterized primarily by insulin resistance – appears in "up to one-third of hypertensive patients." "Visceral obesity, insulin resistance, oxidative stress, endothelial dysfunction, activated renin-angiotensin system, increased inflammatory mediators, and obstructive sleep apnea" all appear to play a role in the progression of hypertension in those with metabolic syndrome. [ref]
Many more scientific articles – supported by substantial evidence – further elaborate on this theory. Some researchers even claim that there is a causal and independent relationship between insulin and essential hypertension. [ref, ref, ref]
[3] – How Does Insulin Affect Blood Pressure?
Insulin inhibits renal sodium excretion and overrides the pressure natriuresis mechanism, which in turn increases blood pressure. [ref, ref, ref, ref, ref] So while excess sodium in the blood slightly raises blood pressure, the problem lies in that insulin prevents the kidneys from excreting the excess sodium, which keeps blood pressure elevated.
Yes, reducing dietary sodium intake will lower the concentration of sodium present in the blood and may marginally decrease blood pressure. Adding ice cubes to an overheated hot tub will cool it down. But this does not address the root issue. In healthy individuals with low levels of circulating insulin, any excess sodium – along with water – is simply excreted in the urine. (Hence why you get thirsty after eating something salty.) This is also why the 24-h urinary sodium excretion measurement is considered the gold standard method for measuring population sodium intake, as any excess sodium consumed is simply excreted in the urine.
[4] – Low Insulin & Hypertension
If insulin truly does play a role in the pathology of hypertension, you would expect that lowering insulin would lower blood pressure. Well, that’s exactly what happens.
Hypertensive diabetics taking exogenous insulin were tested to see how lowering their insulin dosage would affect their blood pressure and sodium excretion. Their dosage was lowered by approximately 20 IU for 6 consecutive days. Prior to the intervention, the mean blood pressure was 171.3/97.3 mmHg, and urinary sodium excretion was 96.0 mEq/L. After 6 days on the intervention, the mean blood pressure fell drastically to 138.2/79.7 mmHg (almost non-hypertensive range for diabetics) and sodium excretion tapered down from 158 mEq/L on the first day, to 105.3 mEq/L on the sixth. (Once again, demonstrating that when insulin is lowered, the kidneys can release more sodium, thus reducing blood pressure, and vice versa.) The authors conclude that there may be a "causal relationship between insulin and blood pressure even in essential hypertension". [ref]
In this dietary based study, a low-carbohydrate diet was tested against a low-fat diet for weight loss over 48 weeks. (Low-carbohydrate diets necessarily lower endogenous insulin secretion, since carbohydrates elicit a greater insulin response as compared to protein or fat.) The authors concluded that "the [low-carbohydrate diet (<20g carbohydrate/day)] had a more beneficial impact than [a low-fat diet] on systolic (−5.9 vs 1.5 mmHg) and diastolic (−4.5 vs 0.4 mmHg) blood pressures." [ref]
[5] – Sugar’s Effect On Blood Pressure
Refined carbohydrates – such as simple sugars and wheat flour – tend to illicit the greatest insulin response of any food. Unsurprisingly, such saccharides are found almost exclusively in processed foods (that coincidentally, may also be salty). As one would expect, they tend to increase blood pressure.
A systematic review of randomized controlled trials reviewed the effects of sugar on blood pressure. In trials over 8 weeks in duration – independent of increases in body weight – the mean systolic blood pressure increased by 6.9 mmHg, and diastolic blood pressure by 5.6 mmHg. [ref]
In this randomized controlled trial, consuming 200g of fructose daily for only 2 weeks lead to a mean increase in systolic blood pressure by 7±2 mmHg, and diastolic blood pressure by 5±2 mmHg. [ref]
This scientific article explains that "high-insulinemic food, typical of current "Western" diets, has the potential to cause hyperinsulinemia and insulin resistance, as well as an abnormally increased activation of the sympathetic nervous system and the [RAAS], alterations that play a pivotal role in the pathogenesis of ... hypertension." [ref]
[6] – Additional Reading
If you are still unconvinced about the insulin hypothesis of hypertension, I’ve included 5 additional scientific articles below that go into much further detail on the topics of salt, sugar, insulin, hypertension and cardiovascular disease. [ref, ref, ref, ref, ref] If you have not read it, I highly recommend "The Salt Fix", by Dr. James DiNicolantonio.
Conclusion
"Officials at Health Canada have determined that the scientific consensus and totality of best evidence continues to support the health benefits that can be achieved by lowering sodium intake." As demonstrated in the present letter, there is NOT a scientific consensus. The totality of best evidence was NOT considered. There is NO meaningful research to support the health benefits from lowering sodium intake.
You’re targeting the wrong suspect. Insulin (not sodium) appears to play an important role – perhaps even a causal role – in the progression of hypertension. High-insulinemic foods – notably refined carbohydrates – should be the focus of dietary restriction for the prevention and treatment of hypertension, not sodium.
"The Department uses the best available evidence to support food and nutrition related policies and regulations. ... Our approach to sodium reduction is consistent with current international efforts of sodium reduction." Prior to your reply, I trusted that Health Canada had a team of expert researchers that critically investigated important health matters. I was unaware, however, that Health Canada does not conduct any of its own research, and simply "copy-pastes" whatever large, international health institutions advise.
I am disappointed that you are not even a little bit intrigued by this alternative hypothesis to hypertension. Instead, you aim to dismiss my arguments and research, and back up your existing beliefs with illogical, inconclusive and unscientific "proof". Science cannot progress if you don’t rethink your current beliefs.
If it’s true that "Health Canada continues to monitor emerging science to keep up to date with the latest evidence and adjust its policies accordingly", I fully expect you to update the sodium guidelines based on this present letter and the research I’ve provided. If you do not personally have the authority to revise Canada’s Dietary Guidelines, please send this letter to those who do have the authority to reassess the guidelines.
I truly hope that we can come to an understanding and that you will take action on this matter, as I am prepared to take legal action if necessary.
The science is NOT settled. The totality of the evidence has NOT been considered. Your belief that excess sodium consumption causes hypertension is WRONG.
Remember that science has been wrong before. Starting in the 1920’s – and for over half a century – doctors were promoting the use of cigarettes, reassuring patients "that smoking was safe". [ref]
Stop blindly trusting "the best available evidence" from large, international health institutions. They’re not infallible gods. They may even be as misguided and uninformed as you are. Start taking your job seriously and maybe someday you will have a real impact on Canadians’ heath.
Anthony Grisé
Health Researcher
P.S. I believe you meant "over time" and not "overtime".

Letter To Health Canada on Sodium Restriction – p.1
December 28th 2020
~ 8 minute read
This letter was addressed to Karen McIntyre, the Food Directorate Director at Health Canada. She sent out an e-mail detailing her mission to reduce Canadians’ sodium intake, due to it’s major risk on heart disease. I disagree with her position that salt is the main culprit in heart disease. In fact, consuming too little salt has detrimental health consequences. So I sent her the following letter.
Subject : Salt : Could Eating More Be Healthier?
Hi Karen,
Limiting Canadian’s salt intake will NOT reduce their rates of heart disease. It will worsen their metabolic health, increase their risk of diabetes and may even increase heart disease mortality.
I respect your dedication towards bettering the health of Canadians. However, if you truly strive to improve people’s health, I think it’s important that you don’t ignore evidence that opposes the status quo of nutrition research. I hope that you will keep an open mind when reading the following letter.
Based on my personal findings and research, the current recommendations to reduce salt intake are not justified – or even healthy. Let me explain.
Firstly, I’d like to disclose that I’m not affiliated with any organization or industry and have no financial interests. Health is a passion of mine. I strive to know true health. I practice what I preach (but don’t mind the occasional treat). I consume generous amounts of salt every day.
Over 60% of Canadian adults consume more sodium than the 2300mg upper limit of the dietary guidelines¹. Yet, only 19% of adults have been diagnosed with high blood pressure². Why doesn’t everyone who exceeds their recommended sodium intake have high blood pressure? What if salt isn’t entirely responsible for high blood pressure?
What if salt isn’t as bad as we thought?
A majority of Canadians are unable to follow a low-salt diet. Their instinctive, primal need for salt drives them to consume more than what is advised. So which do you think is more reliable: the dietary guidelines, or our body’s instinctive craving for salt?
Most people drink less than the recommended 8 glasses of water per day. Rather than rely on an outdated, unscientific recommendation, isn’t it more logical to simply drink when we’re thirsty? Why not rely on our thirst to tell us how much to drink? The same principle should be applied to eating salt. So how much salt should we consume then?
Unlike addictive substances, salt intake is a negative feedback loop. The more salt you eat, the less you crave it. Similarly, the less salt you eat, the more you crave it. Your body regulates it’s cravings for salt based on how much it needs. According to the Sodium Reduction Strategy for Canada, "the current mean intake of sodium by Canadians is about 3,400 mg per day"². Why then would our bodies tell us to eat more salt than is healthy? I would argue that the body’s need for sodium is closer to the current intake than the recommended intake of 2300mg/day (or the 1500mg/day recommended by the Institute of Medicine). Canadians today actually consume much less salt than we did historically.
Throughout history, people consumed much more salt than we do today. "Western societies consumed between 3 and 3.3 teaspoons (15-17 grams) of salt per day from the early 1800s until the end of World War II. ... After World War II, when refrigeration began to displace salt as the main means of food preservation, salt consumption in the US (and somewhat later in other countries) dropped dramatically to about half that rate, or nine grams (1.8 teaspoons) per day."³
Everyone and their dog must have had heart disease back then!
In reality, heart disease was much less common in the beginning of the 20th century than it is now. In 2010, heart disease accounted for 24% of all deaths, whereas in 1900, it was only 8% (US data)⁴.
What about their blood pressure? Surely all the additional salt in their system would be bad for their health!
When you drink too much water, your body will excrete any water it doesn’t need. Same goes for sodium. The excess sodium you ingest is simply filtered out by the kidneys and is excreted in the urine.
Worldwide, the average per-capita consumption of sodium is 3.95g per day, "nearly double the two grams daily recommended by the World Health Organization"⁵. Which do you think is more likely: that a majority of people on earth consume twice as much salt as is healthy, or the WHO’s guidelines underestimate people’s need for salt?
According to this internationnal study on sodium intake and heart health, those who consumed between 4000mg to 6000mg of sodium (10g to 14g of salt) per day had a LOWER risk of cardiovascular events as compared to those that ate more OR LESS sodium. Consuming the recommended 2000mg of sodium per day put you MORE at risk for heart disease than consuming 6 times as much (12000mg/day). Maybe less isn’t better.
This systematic review analyzed 8 randomized controlled trials (the gold standard in nutrition research) on the effects of reducing salt intake for the prevention of cardiovascular disease. In both normal and high blood pressure participants, there was NO significant reduction in cardiovascular disease from limiting salt consumption.
This 2015 study on South Koreans – South Koreans having the lowest rates of heart disease worldwide – found that those who consumed the MOST sodium had the LOWEST blood pressure, rates of heart disease and diabetes. Inversely, those that consumed the LEAST amount of sodium had the HIGHEST blood pressure, rates of heart disease and diabetes. The average consumption of sodium in Korean males is 5300mg/day, almost triple the recommended intake⁷.
Similarly, this study found that blood pressure didn’t change significantly between tertiles of salt consumption. Although blood pressure didn’t change significantly between tertiles, "lower sodium [intake] was associated with higher [cardiovascular disease] mortality".
Humans, like all mammals, require salt – it is an essential nutrient. Elephants, for example, will uproot entire trees just to get at the salty soil under the roots. Some animals will drink urine due to it’s sodium content. Cows require salt licks for optimal health. It’s required for digestion, for bone formation, for nerve impulses and for muscle contraction. The heart (a muscle) requires salt to function properly.
The Sodium Reduction Strategy for Canada states that "high blood pressure is THE major cause of cardiovascular disease", yet I’ve found no research to support this statement. Some studies do show that significantly cutting back on your salt consumption will lower your blood pressure. Yet, most of these studies – including the ones cited in the Sodium Reduction Strategy for Canada – show only a very small reduction in blood pressure. Furthermore, multiple studies show that consuming a low salt diet can actually be harmful for your health.
Those who limit their salt intake are more likely to have high LDL cholesterol, impaired metabolism, greater inflammatory markers, insulin resistance and fatigue ⁸ ⁹ ¹⁰.
There may be an association between salt consumption and heart disease. Nothing more than an association though. It could be explained by the fact that "commercially processed foods account for 77% of [Canadian’s] sodium intake"². Consider that it may not be the salt itself that is responsible for heart disease and high blood-pressure, but the other ingredients contained in the processed foods that may be to blame (sugar, vegetable oils, wheat, etc.).
Salt does not appear to be a significant contributor to heart disease. Furthermore, adopting a low salt diet may even increase your risk of disease, including heart disease. Despite the large consumption of salt in the beginning of the 20th century, heart disease deaths were a third of what they are today. The current hypothesis that consuming more than 2300mg of sodium is the leading cause of heart disease is wrong.
The guidelines on salt consumption need to be revised. You could unintentionally be harming the health of millions of Canadians.
Sources :
1 - https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/sodium/sodium-reduced-targets-2020-2025.html
2 - https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/sodium/related-information/reduction-strategy/recommendations-sodium-working-group.html
3 - https://www.westonaprice.org/health-topics/abcs-of-nutrition/salt-and-our-health/
4 - https://www.ncdemography.org/2014/06/16/mortality-and-cause-of-death-1900-v-2010/
5 - https://www.washingtonpost.com/news/to-your-health/wp/2014/08/14/salt-intake-is-too-high-in-181-of-187-countries-around-the-world/
6 - https://www.nejm.org/doi/full/10.1056/NEJMoa1311889
7 - https://www.who.int/dietphysicalactivity/Elliot-brown-2007.pdf
8 - https://pubmed.ncbi.nlm.nih.gov/1921253/
9 - https://www.sciencedirect.com/science/article/abs/pii/S002604951000329X
10 - https://www.sciencedirect.com/science/article/abs/pii/S0021915008000063
Additional Resources :
a - The Salt Fix, Dr. James DiNicolantonio
b - Salt and our Health (article) - https://www.westonaprice.org/health-topics/abcs-of-nutrition/salt-and-our-health/
c - It's Time to End the War on Salt (article) - https://www.scientificamerican.com/article/its-time-to-end-the-war-on-salt/

Fat Intake & Heart Disease : A Flawed Hypothesis?
September 14th 2020
~ 15 minute read
I recently joined Dr. Matthew Nagra, a plant-based advocate, in a discussion regarding the effects of fat and LDL on Heart Disease. You can find the full video below, as well as my slideshow presentation.
Power Point Presentation (.pdf)
(I won’t be offended if you don’t watch the entire 2 ½ hour video. Matthew rambled on for most of it anyway.)
I’ve also included a much more detailed, supplementary article below further explaining my view of fat intake on heart disease. I tried to make it as simple as possible to understand for those who have a life outside of nutrition research.
Introduction
The idea that fat – especially saturated fat and cholesterol – contribute to heart disease is a relatively new hypothesis. In the early 20th century, heart disease was almost unheard of. Over the following decades, however, heart disease deaths rose steadily, reaching its peak in the 1980’s. In 2007, coronary heart disease was the cause of half of all deaths in the US. [ref] What caused this massive increase in deaths from heart disease? Let’s take a look at the role fat consumption played on heart disease throughout the last century.
How Dietary Fat Became the Villain
Animal fats – known to be high in saturated fat – fell drastically over the 20th century. These fats were gradually replaced with "heart healthy" plant oils, shortenings and margarine. [ref] So, despite saturated fat consumption decreasing over the last century, heart disease on the other hand has been increasing. If anything, there seems to be an inverse association between saturated fat and hear disease.
So how did this hypothesis prevail? Researcher Ansel Keys – not a cardiologist, or even a medical doctor at that – formulated his Diet Heart Hypothesis in the 1950’s. [ref] His controversial "Seven Countries Study" published in 1953 demonstrated a strong association between fat consumption and rates of heart disease. [ref] What Keys left out of his study, however, was that he actually surveyed 22 countries for his analysis. By choosing only the studies that best represented his hypothesis, he was able to show a strong association between fat intake and heart disease. A later review of his study showed that, "The apparent association is greatly reduced when tested on all countries for which data are available instead of the six countries used." In fact, choosing 6 other countries Keys surveyed showed an inverse relationship between fat intake and rates of heart disease. [ref]
Rather than try to explain the reason why some countries that consumed large amounts of saturated fat had low levels of heart disease, they were simply categorized as "paradoxes" and ignored. "The French paradox is the observation of low coronary heart disease death rates despite high intake of dietary cholesterol and saturated fat." [ref] Obviously, Keys left out this country from his analysis.
Consider this : why don’t other carnivores in the wild – such as lions, wolves and bears – get heart disease? Surely their high intake of fatty meat would cause them to die young from heart disease. And yet this isn’t a common occurrence. Interestingly though, when dogs – carnivorous animals in the wild – are fed a plant-based, "heart healthy", legume-rich feed, they develop heart disease. [ref]
Contradictory Evidence
To my knowledge, there is currently no high quality evidence showing that saturated fat intake directly causes heart disease. Associations, sure. But none that specifically isolate saturated fat as a causal factor in heart disease. In fact, there are many high-quality studies that show no effect – or even an inverse effect – of saturated fat and cholesterol intake on heart disease incidence and mortality. [ref] [ref] [ref] [ref] [ref] [ref] [ref] [ref] [ref] [ref] [ref] [ref]
Alternatively, we can look to populations that consume a high fat diet. And counterintuitively – despite their large intake of animal fat and saturated fat – these populations tend to have far fewer cases of heart disease than what is expected. [ref] [ref] [ref] [ref]
A New Culprit for Heart Disease?
Keys later proposed the Lipid Heart Hypothesis, which blames elevated serum cholesterol – notably LDL cholesterol – as the cause of heart disease. Because cholesterol is found in the arterial plaques of victims of heart disease, it must be the culprit. Seems logical enough.
Although LDL is the accused culprit, there are many more villains that play a role – possibly even a bigger role – on heart disease than the accused LDL. Other risk factors that increase heart disease risk include :
- High blood pressure,
- Low HDL,
- High Triglycerides [ref],
- Low HDL & High Triglycerides, [ref]
- Insulin Resistance, [ref]
- Metabolic Syndrome, [ref] [ref] [ref] [ref] [ref]
- Diabetes,
- Alcohol,
- Smoking,
- Obesity,
- Genetics, and a
- Sedentary Lifestyle.
- [ref]
To ignore these other factors – which in combination may predict heart disease much better than simply LDL – is ignorant.
What is LDL Cholesterol Exactly?
LDL stands for "Low Density Lipoprotein". In fact, LDL isn’t cholesterol. LDL is like a bus that carries cholesterol molecules, triglycerides and fat soluble vitamins to various parts of the body. It originates in the liver, where it is sent off to deliver its cargo to cells around the body. In contrast, HDL (High Density Lipoprotein) – considered "good" cholesterol – has the opposite task. HDL collects fat from around the body and brings it back to the liver to be processed. Lipoproteins have the important task of transporting fat – which doesn’t mix well with our water based blood – around the circulatory system. Think oil and water.
Cholesterol on the other hand is nothing to be afraid of. In fact, cholesterol is vitally important for good health. Did you know that the average person produces around 80% of their daily requirements of cholesterol in the liver (800mg/day)? [ref] That’s right, the body manufactures its own cholesterol. The less cholesterol you eat, the more your body produces, and vice-versa. If cholesterol is so deadly and dangerous, why would the body make it in the first place – and so much of it? Breast milk – the preferred food for all growing newborn mammals – is full of cholesterol. [ref] So, what is all this cholesterol used for in the body?
Cholesterol is vital for life and serves a multitude of functions in the body :
- It is a crucial component of every cell membrane in your body,
- It aids in cell reparation,
- It helps fight off viral and bacterial infections, [ref] [ref] [ref]
- It makes up the myelin sheath that surrounds and insulates nerve cells,
- It is necessary for the synthesis of many hormones (estrogen, testosterone, cortisol, Vitamin D…),
- And it even may be protective against heart disease. [ref]
In fact, the brain is so dependant on cholesterol, that it has its own cholesterol production centre. Despite only contributing 2% of our body weight, the brain uses 25% of all cholesterol in the body. [ref]
The 2015 US Dietary Guidelines' Scientific Report even stated that, "consistent with the conclusions of the AHA/ACC report, cholesterol is not a nutrient of concern for overconsumption". [ref]
Why LDL Is Thought to Be Linked to Heart Disease
What makes this LDL "bus" a risk factor in heart disease? A number of large studies have shown a strong association between levels of LDL and risk for heart disease. Therefore, because saturated fat raises LDL, and LDL is associated with heart disease, saturated fat causes heart disease! Case closed.
In practice however, this isn’t necessarily the case. In fact, people admitted to the hospital for heart disease tend to have normal or even low levels of LDL cholesterol. [ref] So why do these people with low LDL still get heart disease?
A theory as to why this might occur is that LDL levels drop in people who recently had a heart attack. Yet, I haven’t found evidence to support this claim.
What Makes LDL Go Up?
Logically, if you’re eating more fat, your body has to process more fat. Especially in the case of a low-carb diet, the cells of your body become more reliant on fat – as opposed to carbohydrates – as a source of fuel. To feed these hungry cells, LDL is sent off with its fatty cargo around the body to supply cells with nutrients and energy. LDL then returns to the liver where it is removed from circulation, recycled and ready to deliver more cargo when needed.
Although LDL may go up in the case of a low-carb diet, this isn’t the only factor that can increase LDL. Probably the most common reason for elevated LDL outside of the context of a low-carb/high-fat diet is damage to the LDL. If LDL is damaged, it can no longer do its job and isn’t even recognized by liver anymore (so isn’t taken out of circulation by the liver). This damaged LDL accumulates in the blood, while the body produces even more LDL to make up for the damaged LDL. Hence, higher LDL.
Other than saturated fat intake, LDL can go up due to :
- Low HDL,
- Inflammation,
- Stress, [ref] [ref]
- Diabetes,
- Smoking,
- Alcohol,
- Obesity,
- A Sedentary Lifestyle, and
- Trans Fats [ref].
It’s much more likely – in studies showing a positive correlation between LDL and heart disease – that LDL is elevated not in the context of a high-fat/low-carb diet, but because of other lifestyle factors. Why would context matter?
Why can’t we assume that everyone with elevated LDL has a similar risk for heart disease?
Context Is Crucial to Consider
It’s common in the field of research to translate findings from a small group of people to the entire population. It’s often done for practical and financial reasons, since it would be much more difficult and expensive to study every single person in a given population and to consider all potential variables. Is this really representative of the entire population?
Take the sleeping pill "Ambien" for example. There were many cases of women who had taken the drug and crashed their car the following morning. "The problem wasn’t entirely the drug itself, but the dosage. … It turns out that women metabolize the active ingredient in Ambien twice as slowly as men." Meaning that the drug was still in their system the following morning, whereas in men it had worn off by then. The reason for this discrepancy is that "the clinical trials on Ambien focused on male test subjects."
"If they’re using this hypothetical, average man and they’re basing dosage on it, that’s kind of scary. Not just because it doesn’t apply to women, but because it also doesn’t apply to a lot of men either", Diana Zuckerman, president of the National Center for Health Research states. "Data from women is often mixed in with data from men, which can hide sex specific reactions to medicine." Zuckerman also mentions that "The FDA (Food and Drug Administration) [is] making the decisions about what medications are being sold … and they are not required to include women, people of color, people over 65." The reason why certain demographics are excluded from studies is because "the more people you study, the more it costs to do the research." [ref]
Context is crucially important to consider when conducting research. To my knowledge, there has not been a quality study that has been conducted that demonstrates that high LDL – in the specific context of a low-carb/high-fat diet – increases your risk for heart disease. In this demographic, elevated LDL may not have the same effect on heart disease risk as those in the general population.
LDL Results Aren’t That Accurate
On a standard blood test, LDL is measured by its volume in the blood – referred to as LDL-C (low-density lipoprotein concentration). In fact, LDL itself isn’t even measured, but calculated using other lipid markers using the following equation.
- LDL-C = (Total Cholesterol) - (HDL) - (Triglycerides / 2.17) mmol/L [ref]
Imagine that we each have a jar filled with marbles. In this example, marbles represent LDL. The fuller your jar is, the higher your LDL-C is. But this metric tells us very little about the contents of the jar. How many marbles are in each jar? Are the marbles big or small? Are the marbles smooth or bumpy? Using this analogy, your jar could be less full, but have more marbles in it since most of them are small. And what if small marbles were less desirable than larger marbles? In this example, you could actually have more, undesirable marbles than I do, even though my jar is fuller.
In the same order of ideas, there are in fact 2 types of LDL : Pattern A (also described as "large, buoyant" LDL) and Pattern B (also described as "small, dense" LDL).
Standard blood tests aren’t able to distinguish Pattern A or Pattern B particles. So, in theory, you could have the same LDL-C score as someone else but have wildly different amounts or patterns of LDL particles. [ref]
Good and Bad LDL
The reason why people with relatively low LDL-C may still develop heart disease might be due to their LDL Pattern. Pattern B LDL seems to be much better associated with heart disease than Pattern A LDL. [ref] [ref] [ref] [ref] Meaning that even if you have relatively low LDL-C, the majority of your LDL could potentially be Pattern B LDL, increasing you risk for heart disease.
The difference between Pattern A and Pattern B LDL can be measured by their size (by a few nanometers only). More importantly though, Pattern A LDL consists of normal, healthy LDL particles whereas Pattern B LDL consists of abnormal, damaged LDL particles.
Many factors can damage LDL and increase levels of Pattern B LDL :
- A High-Carbohydrate Diet, [ref]
- Free-Radicals,
- Trans Fats, [ref]
- Smoking,
- Diabetes, [ref] [ref]
- Metabolic Syndrome, [ref] [ref] [ref]
- Toxins, and
- Stress. [ref] [ref]
What about saturated fat? Although saturated fat does increase levels of LDL-C, studies show that most of this LDL is Pattern A – posing less of a risk for heart disease. [ref] [ref]
As Dr. Paul Mason explains, "Saturated fat makes LDL high, but sugar makes LDL bad".
Alternative Hypotheses
The exact pathology of how and why LDL accumulates in the arterial walls is still not fully understood, but there are a few hypotheses.
One hypothesis suggests that the endothelium – the protective lining of the arterial wall – becomes eroded due to high blood sugars and/or Pattern B LDL. The exposed arterial wall then becomes inflamed and damaged. LDL brings cholesterol to the damaged artery and "patches" the damaged area to allow it to heal – similar to a scab on a wound. In this scenario, blaming the cholesterol "patch" for heart disease is akin to blaming the scab for the cut, the blister for the burn, or the fireman for the fire. They’re always present at the scene of the crime, so its easy to lay the blame on them.
Another hypothesis suggests that because Pattern B LDL cannot be removed from the circulation by the liver (because it’s damaged and is no longer recognized by the liver), macrophages within the arterial wall "consume" these damaged particles which then build-up over time in the arterial wall.
Pattern B LDL may not even have a direct role in the progression of atherosclerosis. It could simply be a marker for cardiovascular ill-health. Again, the exact pathology isn’t fully understood, but taking into consideration Pattern A and Pattern B LDL in the progression of heart disease may better explain some of the logical fallacies and inconsistencies currently present in the traditional Lipid Heart Hypothesis.
Better Markers for Heart Disease Risk
So rather than relying on LDL-C, what metrics can be used to better predict heart disease?
A factionary test can determine if your LDL is mostly Pattern A or Pattern B. Another quality test to identify risk of heart disease is the Coronary Artery Calcium score (CAC). [ref] [ref] [ref] This test visually identifies plaque progression in the arterial walls. No guessing needed – the fewer plaque growth in the arteries, the better. Although there has not been any large study specifically looking at CAC scores among those following a low-carb/high-fat diet, there are a few cases of long term adherers of an animal-based diet that show a perfect score of 0. [ref] [ref]
These aren’t very common tests and could be expensive or unavailable. However, two standard blood test results – triglycerides and HDL – could give you a good idea of your level of Pattern B LDL. Low levels of HDL and high levels of triglycerides are shown to be inversely associated with levels of Pattern B LDL. [ref]
So to summarize, if you are following a low-carb diet, are metabolically healthy, have high levels of HDL, low levels of triglycerides, and limit lifestyle factors that increases your Pattern B LDL, it’s unlikely that you will develop heart disease any time soon – even if your LDL high.
*This article is not meant to be medical advice.
- Anthony Grisé